Introduction
The biobetters market is increasingly recognized for its potential to reduce overall healthcare costs. Biobetters, improved versions of existing biologics, are designed for enhanced efficacy, safety, and patient convenience. Their adoption can lower direct and indirect healthcare expenses by reducing hospitalizations, minimizing adverse events, and improving treatment adherence. As chronic diseases, oncology, and autoimmune disorders continue to place a heavy financial burden on global healthcare systems, biobetters provide a sustainable solution. By offering longer-lasting effects, fewer side effects, and more predictable outcomes, these next-generation biologics optimize resource utilization and contribute to economic efficiency for healthcare providers, payers, and patients alike.
Direct Cost Reduction Benefits
Lower Hospitalization Rates
Enhanced efficacy of biobetters reduces disease exacerbations and complications, leading to fewer hospital admissions and shorter stays.
Reduced Adverse Events
Biobetters are engineered to minimize immunogenicity and side effects, decreasing the costs associated with managing treatment complications.
Fewer Treatment Failures
By providing more consistent therapeutic outcomes, biobetters reduce the need for switching therapies, repeat treatments, or additional interventions.
Optimized Dosage and Administration
Longer half-life and improved formulations allow fewer doses, lowering costs related to drug administration and patient monitoring.
Indirect Cost Savings
Improved Patient Productivity
Patients with stable disease management experience fewer missed workdays, contributing to broader economic savings.
Reduced Caregiver Burden
Simplified treatment regimens and better tolerability reduce the time and resources spent by caregivers.
Preventive Health Impact
Early and effective biobetters prevent disease progression, avoiding more expensive interventions in the long term.
Enhanced Healthcare Resource Utilization
Less strain on hospital beds, staff, and medical equipment allows more efficient allocation of healthcare resources.
Impact Across Therapeutic Areas
Oncology
Biobetters in cancer treatment improve patient survival and reduce chemotherapy-related complications, lowering overall treatment costs.
Autoimmune Disorders
Improved biologics reduce disease flares, hospitalizations, and long-term complications, reducing chronic care expenditures.
Diabetes and Chronic Diseases
Long-acting biologics improve glycemic control and cardiovascular outcomes, lowering hospitalization and emergency care costs.
Rare and Orphan Diseases
Biobetters designed for rare conditions reduce long-term care costs by providing effective, targeted therapy.
Role of Clinical Efficacy
Evidence-Based Cost Reduction
Clinical trials demonstrate that biobetters outperform originators in efficacy and safety, validating potential cost savings for payers and providers.
Real-World Evidence
Patient registries and electronic health records show reduced healthcare utilization, reinforcing economic benefits.
Personalized Therapy
Targeted biologics improve outcomes, reduce unnecessary interventions, and prevent overtreatment, driving efficiency in healthcare spending.
Treatment Adherence
Enhanced safety and simplified dosing increase adherence, reducing long-term complications and related costs.
Payer and Policy Considerations
Reimbursement Strategies
Insurance coverage of biobetters is increasingly justified by demonstrated cost savings and superior patient outcomes.
Value-Based Pricing
Linking cost to clinical outcomes ensures that biobetters provide measurable economic benefits while maintaining market sustainability.
Government Support
Policy initiatives encourage adoption of biologics with proven cost-effectiveness, particularly in chronic and high-burden diseases.
Incentives for Healthcare Providers
Providers adopting biobetters benefit from lower readmission rates and improved performance metrics, reinforcing broader systemic savings.
Manufacturing and Supply Chain Efficiencies
Advanced Bioprocessing
Optimized production methods reduce waste, improve yield, and decrease manufacturing costs, indirectly contributing to lower healthcare expenses.
Local Production
Regional manufacturing reduces distribution costs and ensures faster access to therapies, avoiding delayed treatment complications.
Cold Chain Optimization
Efficient storage and transport prevent product degradation, ensuring patients receive effective treatment without additional medical interventions.
Strategic Partnerships
Collaboration with contract manufacturing organizations accelerates production timelines and reduces resource utilization.
Global Market Implications
Developed Economies
Biobetters reduce long-term costs in high-expenditure healthcare systems, particularly for chronic and complex diseases.
Developing Nations
By preventing complications and improving adherence, biobetters reduce healthcare strain and out-of-pocket expenses in resource-limited settings.
Healthcare System Sustainability
Adoption of cost-effective biobetters supports sustainable healthcare financing by optimizing resource allocation and reducing financial burden.
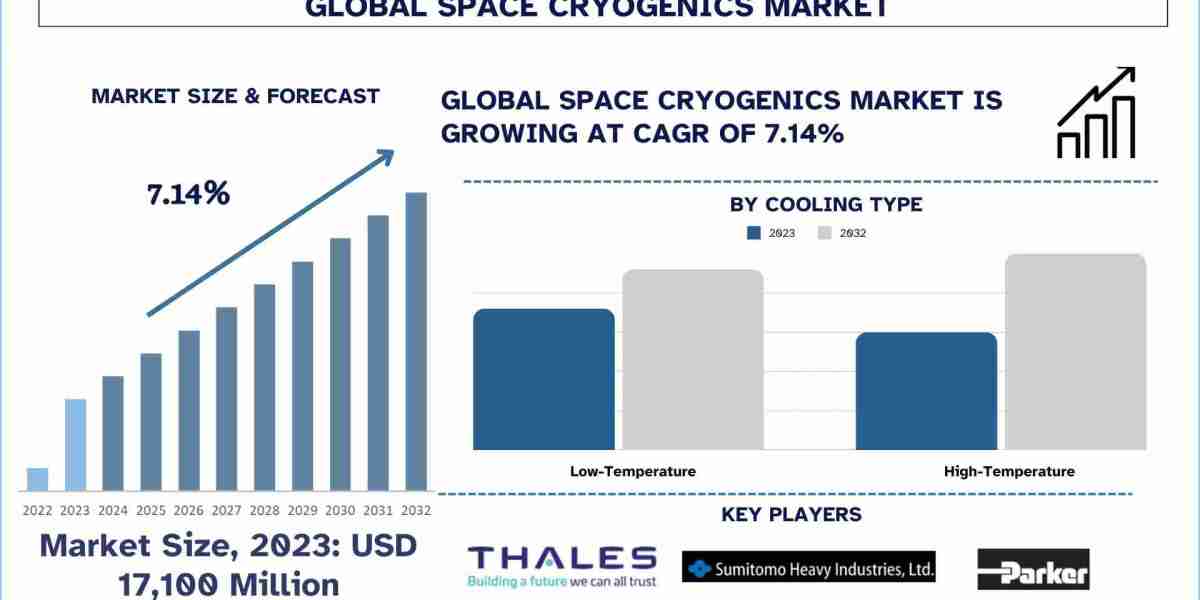
Economic Forecast
As adoption increases, biobetters are expected to contribute significantly to healthcare cost containment, improving access and affordability.
Future Outlook
By 2030, the biobetters market will play a critical role in global healthcare cost reduction. Increasing availability of real-world evidence and clinical validation will strengthen payer confidence and policy support. Integration of AI and big data analytics will help monitor cost savings, optimize treatment protocols, and improve patient outcomes. Expansion into emerging markets, coupled with innovative pricing and reimbursement strategies, will make biobetters a cornerstone of sustainable healthcare. Companies that demonstrate both clinical and economic value will achieve faster adoption, ensuring improved patient care while reducing financial pressure on healthcare systems worldwide.
Conclusion
Biobetters represent a transformative opportunity in healthcare by delivering next-generation biologics that improve safety, efficacy, and patient adherence while reducing overall costs. Direct benefits include fewer hospitalizations, reduced adverse events, and optimized dosing, while indirect benefits extend to improved patient productivity, decreased caregiver burden, and more efficient use of healthcare resources. Across therapeutic areas such as oncology, autoimmune diseases, chronic illnesses, and rare conditions, biobetters reduce treatment failures and prevent long-term complications. Adoption is further supported by payer incentives, value-based pricing, government policies, and advanced manufacturing. By focusing on both clinical outcomes and economic efficiency, biobetters are positioned to drive sustainable, cost-effective healthcare solutions worldwide.